Adderall Treatment
Adderall (dextroamphetamine and amphetamine) is a prescription stimulant that is used to treat attention deficit hyperactivity disorder (ADHD) and narcolepsy. Although doctors prescribe it to manage these conditions, Adderall is also commonly misused and abused for its desirable effects. It is estimated that around five million Americans misuse prescription stimulants such as Adderall. Adderall abuse can progress to an addiction, which is characterized by an uncontrollable pattern of Adderall use regardless of negative consequences. While it may be difficult to quit abusing Adderall on your own, luckily addiction treatment can help.

Signs and Symptoms of Adderall Addiction
There are several physical and behavioral symptoms that a person who is addicted to Adderall might display. These symptoms are similar to those of methamphetamine addiction. By recognizing them, you can understand when to seek help.

Some signs of Adderall addiction and abuse may include:
- Rash or hives
If you notice any of the above changes in someone you care about, it’s possible they’re struggling with an Adderall addiction. They don’t have to struggle alone, though—professional help is available. Call us at 1-800-429-7690 to find a rehab program that’s right for them.
Besides the physiological and mood-related signs of Adderall addiction, there are also several behavioral symptoms to be aware of—whether in yourself or someone you know. Some behavioral signs of Adderall addiction include:
- Giving up important social or recreational activities to use Adderall
- Regularly using Adderall in hazardous situations
- Using Adderall despite inability to fulfill obligations at home, work, or school
- Experiencing strong cravings for Adderall
- Wanting to quit or cut down on Adderall use but inability to do so
- Using higher or more frequent doses of Adderall than originally intended
- Spending an inordinate amount of time obtaining Adderall, using it, or recovering from the high
- Continuing to use Adderall regardless of interpersonal issues caused or worsened by use
- Continuing to use Adderall despite physical or psychological issues caused or worsened by use
- Needing higher or more frequent doses to get high (tolerance)
- Experiencing unpleasant Adderall withdrawal symptoms when you abruptly quit
Who is at Risk of an Addiction?
In the United States, controlled substances such as Adderall have a much higher risk of resulting in addiction. According to research, the population most at-risk for Adderall misuse and addiction is young adults between 18 and 25 years of age.
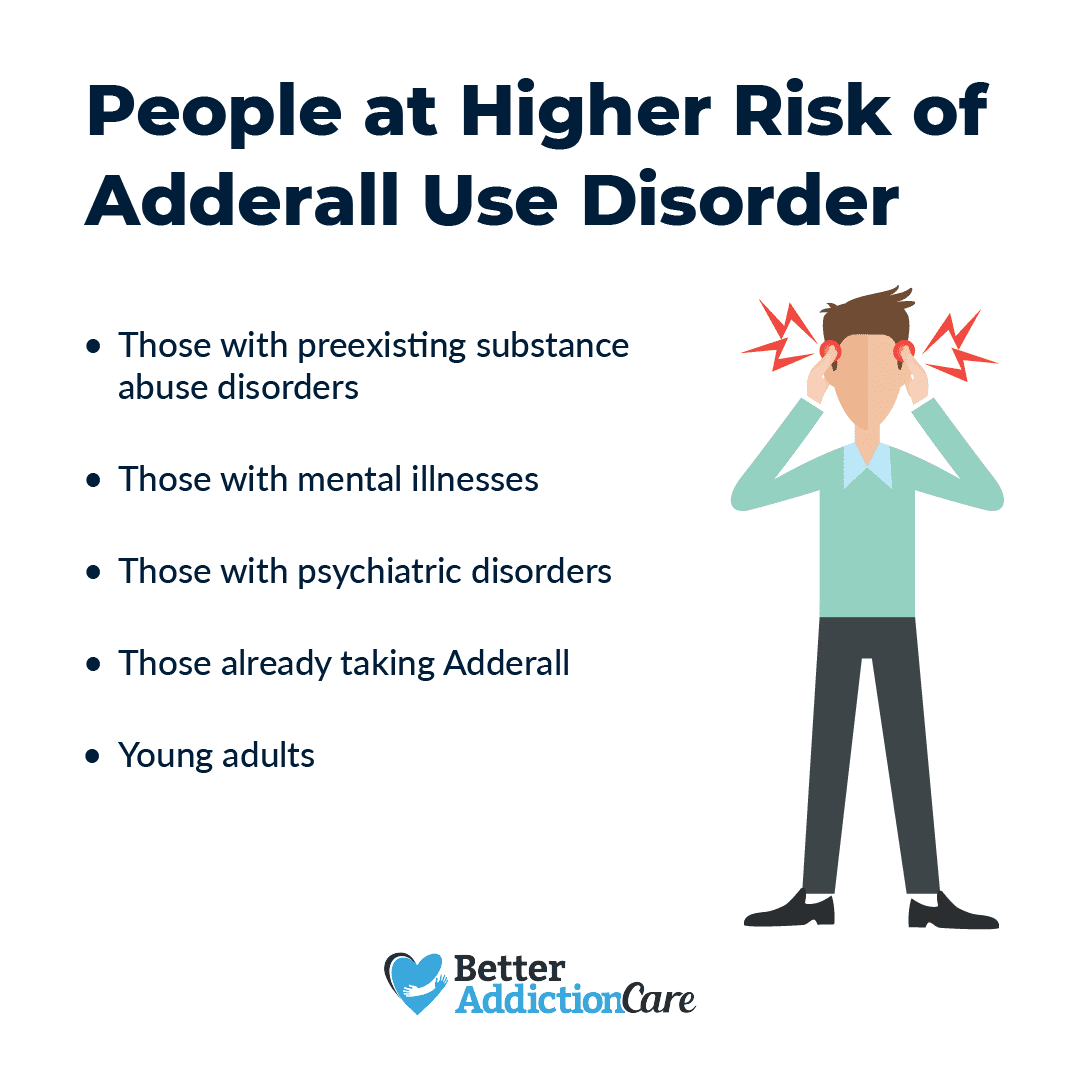
Studies have also shown that higher-risk individuals include people with:
- Other substance addictions
- Mental health conditions, such as anxiety, depression, and bipolar adisorder
- Family history of addiction
- Family history of mental illness
- History of experiencing physical, sexual, or emotional abuse
- History of experiencing neglect
Adderall is most abused by recreational users. However, that doesn’t mean those with a valid prescription cannot develop an Adderall addiction by taking additional dosages or dosages larger than prescribed.
One thing that’s important to remember is that just because you have some risk factors for an Adderall addiction or addiction to any other substance, it doesn’t necessarily mean that you’ll develop one. These risk factors simply increase the chance of becoming addicted to Adderall. But ultimately, if you take your prescription exactly as prescribed or if you avoid misusing this stimulant, then your risk is much lower.
How to Treat Adderall Addiction
When you’re struggling with an Adderall addiction, it can feel like the only way to get through the day is to misuse this stimulant. Unfortunately, this is a self-defeating cycle that can be difficult to end. Here are some tips to help you navigate through the treatment process.
The first step in the healing process is enrolling in a supervised detox program. During Adderall detox, you will be monitored 24/7 throughout the entire process while receiving treatment to mitigate distressing Adderall withdrawal symptoms.
Once the detox phase is complete and you are medically stabilized, you will transfer into an Adderall addiction treatment program—either inpatient or outpatient. Inpatient is the most intensive option that provides you with around-the-clock treatment and care, whereas outpatient involves attending therapy sessions at a facility and then returning home in the evening. Outpatient provides you with less support and structure, so it’s likely a better option if you are highly motivated to quit and have a strong support system.
An Adderall addiction treatment program usually incorporates a variety of therapies and interventions, including:
- Cognitive behavioral therapy
- Family therapy
- Medication management
- Group counseling
- Drug education classes
- Support group meetings
Aftercare and Ongoing Support
Once you’ve successfully completed your Adderall addiction treatment program, you’ll want to consider your options for aftercare and ongoing support. While some may choose to attend Narcotics Anonymous (NA) meetings, others may opt to enter a sober living home.
Sober living programs provide a safe and structured environment, which may be the most beneficial option for those who aren’t ready to fully transition back into their old environment. Every sober living home has different rules, but one rule they all have in common is that you cannot use Adderall or any other substances. These programs may also help you obtain a job.
Other options for aftercare and relapse prevention include:
- SMART Recovery meetings
- Individual therapy
- Step-down care at an outpatient facility
Common Questions About Adderall Treatment
No, not always. If you are prescribed Adderall for a condition, then you will likely develop dependence over time. A dependence on Adderall simply means that your body has adapted to the presence of this prescription stimulant. In the event that you decide you want to stop taking Adderall, speak with your doctor first. They will create a tapering schedule in which you gradually wean off of Adderall to prevent the emergence of withdrawal symptoms. Conversely, if you misuse Adderall, a dependence could lead to the development of an Adderall addiction.
Yes, Adderall is highly addictive, particularly if you misuse or abuse this prescription stimulant to get high, help you focus, or to enhance the high of another substance.
If you or a loved one addicted to Adderall, seeking Adderall addiction treatment is the best course of action. A rehab program can help you quit using Adderall and build the coping skills you need to obtain and maintain abstinence. If you aren’t sure where to start, call our helpline at 1-800-429-7690 to find the right rehab for you.
When taken therapeutically, by someone with ADHD, Adderall helps them focus better. Conversely, if someone without ADHD takes Adderall, they may experience increased energy levels and euphoria, as well as potentially dangerous side effects, such as heart attack.
Yes, abusing Adderall can affect your skin, including premature aging of the face. Studies have shown that amphetamines can significantly impact the body’s aging process, including aging of the face.
Adderall should not be taken recreationally because of its many harmful side effects, both short-term and long-term. Misusing Adderall increases your risk of heart attack, stroke, and sudden death.